 Indexed in Index Medicus and Medline
Indexed in Index Medicus and Medline
Legends in Urology
Richard Turner-Warwick, CBE
MSc, MCh, DM (Oxon), DSc (Hon),
FRCP, FRCS, FRCOG, FACS (Hon), FRACS (Hon)
Emeritus Surgeon, The Middlesex Hospital, London W1 (now UCL)
Emeritus Surgeon, Institute of Urology Hospitals Group, WC1 (now UCL)
Visiting Consultant Urologist, The Royal Prince Alfred Hospital, Sydney
I feel greatly honored to be invited to contribute to the legend series - but I do not feel mythological. I am acutely aware of the immense amount that I owe to so many friends and colleagues along the way, both senior and junior - none more so than my lady wife Margaret. We met at Oxford in 1943 as contemporary medical students in the dark days of the war and married in 1950 when we qualified - we have integrated and supported each other ’s full- time professional lives ever since. She became the Professor and Dean at the Cardio-Thoracic Institute at the Royal Brompton Hospital and eventually President of the Royal College of Physicians (5 years’ hard labor and the first lady president in 485 years of its history). She was appointed a Dame (DBE) in 1991. Many of the facets of our life are recorded in her thoughtful book ‘Living Medicine’ that she wrote for, and gave to, the RCP - it is only obtainable from there (441 (0) 207 935 1174). We have two lovely daughters, one a professor of medicine and the other a teacher, an artist, and now a grandmother - whether we managed to look after them properly is somewhat questionable, but certainly we were deeply indebted to the ever-caring presence and support of my mother who lived next door.
My father was a consultant general surgeon at The Middlesex, one of the large teaching hospitals in London - he specialized in colonic surgery and in varicose veins. He had a particularly inquiring mind and, among many other things, he was the first `to identify the critical importance of the valves of the perforating veins. My mother was also a doctor and was a remarkably good mechanic - before I was 10 she taught me how to dismantle a car engine down to the big-ends and to reassemble it. My grandfather was a dentist and did excellent wood and silver work - I spent many happy hours working with him in his small but well-equipped workshop, making many things. I still have the sophisticated oscillating, double action, twin cylinder steam engine that I machined out of bits of solid brass while at school at Bedales. The acquisition of these various mechanical skills contributed greatly to my surgery - in addition I was able to design and make the various instruments that I developed when I felt the standard issue had improvable shortcomings.
I was most fortunate to be admitted to Oriel College to read medicine at Oxford in 1942 - I still wonder how I managed to achieve this. After my 2 preclinical years I was again most fortunate to be one of the small number seconded to take the academic third year during the war, the Final Honor School of Physiology - I became particularly interested in the correlation of structure and function. With the end of the war I was able to spend a fourth year at Oxford as an anatomy demonstrator, working on the central connections of the Olfactory System of the rabbit with Prof. Le Gros Clark and writing an MSc thesis. I was elected captain of the Oxford rowing crew in 1946 (President of the OUBC) and we won the first Oxford and Cambridge Boat Race after the war.
I then became a clinical medical student and the Broderip scholar at The Middlesex Hospital and qualified in1949. My surgical tutor was Rex Lawrie who had served as a plastic surgeon in the RAMC - before the war hehad obtained the specialist qualifications of both surgery (a Mastership of Surgery and the FRCS) and of internalmedicine (a postgraduate Doctorate of Medicine and the FRCP). This exceptional achievement became my ambitionafter my qualification in 1949 - naturally obtaining this double qualification took me quite a time. In those daysthe training system of a surgeon in England was very different from that in Canada and the USA - it was up to theindividual to choose, and then to apply and compete for, a series of separate house jobs and registrar appointmentsthat would enable one to achieve the desired specialist qualifications. I was able to obtain a consecutive series of training posts in general surgery and, after that, also in orthopedic, urological, colo-rectal gynecological, thyroid, and cardio-thoracic surgery - plastic surgery was a particular interest. This was followed by a considerable time in gastro-enterological medicine with Sir Francis Avery Jones and nearly 2 most valuable years in Professor Robert Scarff’s surgical histology laboratory. Such a breadth of medical and surgical experience is no longer obtainable- some might regard it as excessive but for me it was invaluable. During this time I passed both the FRCS and the MRCP examinations - later adding the FRCP and also the FRCOG. I then became senior registrar to Sir Eric Riches and Ossie Lloyd Davies in urology, gastro-intestinal and colo-rectal surgery for 4 years - in the British system this is a long apprenticeship that is approximately the equivalent of a superannuated nonresident senior resident. During this time I was elected to a Hunterian Professorship at the RCS on the basis of my postgraduate Doctorate of Medicine thesis on the Lymphatics of the Breast (Brit J Surg 46 574).
Following this I was awarded The Middlesex Travelling Fellowship in 1958. I was most fortunate to be appointed a Research Fellow at the Columbia Presbyterian Medical Center in New York where, owing to the illness of the senior resident in urology at the Francis Delafield Hospital, I was asked to stand in for him for 5 months to fill the gap in the training system. During this time, at short notice and quite unexpectedly, I was invited to present a paper on the scrotal drop-back posterior bulbar urethroplasty at the annual meeting of the GU Surgeons at Seaview in 1959 - this was based on a submission I had just made for its publication (J Urol 83 416). An extraordinary opportunity for a senior resident to meet ‘all the greats in the States’.
Perry Hudson, for whom I worked, had trained at the Johns Hopkins Hospital - most caringly, he felt that my quite extensive urological education was lamentably deficient! The financial restrictions in England at that time had limited my travel allowance to only $500 for the year so he contacted a number of his Alumni friends. He made special arrangements with WW Scott for me to be a supernumerary assistant to his senior resident at Johns Hopkins and live in the Brady Institute ‘for free’ for 5 weeks. He then arranged for me to live at home with Hartwell Harrison and work with him at the Peter Bent Brigham for 2 weeks, followed by a similar arrangement at home with Wyland Leadbetter at the Memorial Hospital and again with Dick Alt at the North Shore Hospital - each for 2 weeks and at zero personal expense; incredibly generous. I bought a bright red Ford V8 convertible for the princely sum of $200 with the welcome remuneration of my senior residency. Margaret was working on her PhD thesis in London at the time and wished to visit a number of colleagues - she came over and we drove across the States with a number of academic stopovers on the way. As arranged by Perry, we stayed and visited with CV Hodges and John Barry in Portland, then down the redwood highway to stay with Willard Goodwin in Los Angeles for a week and on to Frank Hinman in San Francisco. We then shared a nonstop drive back to New York in 3 days - we were both very tired when we arrived. We sold the car for $200 before we sailed home on the New Bremen. Was there ever such a privileged and generous introduction to so many of the master urologists in the States who naturally became close friends?
Upon my return to the UK I wrote my Mastership of Surgery thesis and was appointed RSO to Sir David Innes Williams and Howard Hanley at St. Peter ’s Institute of Urology. I was then appointed to the consultant staff of The Middlesex as a general surgeon with charge of the thyroid clinic. When Sir Eric Riches retired in 1963 I was able to develop a specializing urological unit at The Middlesex. My outstanding senior registrar, Euan Milroy, was appointed a second consultant urological surgeon - he took over the care of our urinary tract tumors, the thyroid and parathyroid clinic together with much departmental administration. I was most grateful for this because it enabled me to subspecialize and concentrate exclusively on the development of functional reconstruction which was largely an ‘unwritten book’ at that time. Many of the then-current concepts of functional behavior of the urinary tract were clearly questionable or untenable but the objective reassessment of these required complex urodynamic evaluation which was not available at that time. Working closely with my senior radiological colleague, Graham Whiteside, we set aside a room in his department that was dedicated to cystography. Using the newly introduced image intensifier (initially with only a 7 inch screen) we recorded the image on 35 mm cine film for a weekly team review of all cases - the first full time routine clinical urodynamic service anywhere, it became known as the ‘cine clinic’. However it soon became apparent that, without a synchronous record of both the detrusor pressure and the flow rate, much information that was critically important to diagnosis was lost. Patrick Bates, our urological registrar, became our first Research Fellow. He developed an effective, if primitive, system superimposing a video record of a polygraph that showed the subtracted detrusor pressure and the flow rate onto a split cystographic screen to become the video pressure flow cysto urethrogram VPFCU (BJU 42 714) - the forerunner of modern urodynamic equipment.
Thus in 1968 our Cine Clinic became the first Urodynamic Clinic - a most important ongoing teaching, learning and research function based on the evaluation of more than a thousand symptomatic male and female patients a year. Relatively few urologists shared our interest in detailed urodynamic evaluation initially, however 10 years later the January 1979 volume of Clinics of North America was ‘Clinical Urodynamics’ - a landmark publication that was in fact largely written by our small Clinic in South Britain. This was an innovative exposition of the function and dysfunction of the various components of the urinary tract - it is still remarkable reading. It is now widely recognized that the reliable resolution of many complex vesicourethral dysfunctions requires detailed urodynamic evaluation and this became a required element of the FRCS Urol when this was created in 1986.
We owe a great debt of gratitude to Chris Chapple who further developed the VPFCU as an electronic clinical procedure while he was our research fellow (FRFUT Chapter 14). He was then our senior registrar for 4 years before becoming a consultant at Sheffield - the first urological surgeon to be specifically appointed to specialize exclusively in reconstruction. Naturally he still does his own VPFCUs as part of his diagnostic routine.
The main focus of my personal surgical interest between 1965 and 1990 was the development of substitution and anastomotic procedures for the resolution of strictures of the male urethra from the deep glans split neomeatoplasty for hypospadias (Clin N Amer 6-3 643) to complex traumatic injuries (Brit J Surg 54 55) - our partial-pubectomy repair of 619 pelvic-fracture urethral strictures was reported at the annual meeting of BAUS in 1990. The breadth of specialist training in all three compartments of the female pelvis developed into the horizontal specialty of pelvic surgery which included bowel substitution of the bladder, of the vagina and the resolution of the complications of hysterectomy. Colonic surgeons naturally use a wrap of the conveniently adjacent omentum to reinforce their anastomoses - appropriate procedures for the mobilisation of its vascular pedicle had to be developed to enable short omental aprons to reach and support the closure of ‘simple’ post-hysterectomy vesico-vaginal fistulae to provide a success-rate approximating to 100%. ‘Complex’ childbirth fistulae caused by obstructed labor are quite different because there is usually concomitant damage to the sphincter mechanism - thus although one can almost always close even the largest fistulous defect with the mobilized omentum incontinence may persist (chapters 4 and 12 of FRFUT).
We had a special interest in the problems of female incontinence but rather deferred publicizing this for fear of swamping our small clinic. Eventually, in 2002, I wrote ‘Functional Reconstruction and Gynaeco-Urology’ with Chris Chapple together with some 1500 outstanding illustrations by Paul Richardson. Sadly the printed version of this volume is no longer obtainable but, thanks to the most generous help of one of our retired trainees, we now have all the advantages of an interactive online digital publication of ‘Functional Reconstruction of the Female Urinary Tract’ (FRFUT) at http//rturnerwarwick.com//. As a contribution to teaching and learning we have made this freely available for viewing by all qualified physicians and medical personnel, world-wide and without any charge.
Unlike uro-gynaecological texts, this urological contribution relates to each of the functionally distinct sections of the whole length of the tract with a detailed consideration of practical surgical techniques - the underlying basis of individual minimal-access procedures. The treatment of incontinence should be based upon a proper understanding of continence - the widespread conceptual belief that pelvic floor support of the urethra is essential for the maintenance of its sphincteric competence is unrealistic. Normal continence is entirely dependent upon the independent occlusive function of the intrinsic urethral sphincter - a normal sphincter does not require adjuvant support by the pelvic floor. The competence of a normal sphincter is not compromised by its vaginal prolapse - many entirely continent multiparous ladies have a degree of vesico-urethral descent that enables the whole length of their unsupported urethra to be openly visible at the introitus. Pelvic floor exercises cannot effectively re-elevate a urethral mechanism once it has prolapsed - they are correctly prescribed for mild incontinence because they also exercise and strengthen the all-important intrinsic sphincter due to their common innervation. Stress incontinence is due to varying degrees of weakness of the intrinsic sphincter. When the sphincter mechanism is both weak and prolapsed an efficient urethral elevation procedure (which may or may not involve redeployment of the pelvic floor) is sufficient to restore the competence of the weak sphincter in about 80% of patients - however this simple incontinence procedure has an inevitable overall failure-rate of 15-20% when the sphincter is particularly weak. All these parameters are analysed in chapters 7 & 9 of FRFUT. I had a special interest in an endeavour to restore the competent occlusive function of the residual intrinsic muscle of these particularly weak sphincters by a posterior-approach reduction-sphincteroplasty, using a trans-vaginal access with the patient in a prone position. In appropriate cases we had considerable success with this - both Chris and I use this as a component of our procedure for urethral diverticulectomy. In a small proportion of cases the posterior wall of the urethral sphincter becomes diaphanously thin as a result of childbirth or ageing - the residual anteriorly-eccentric sphincter muscle can be redeployed circumferentially, creating a smaller lumen that can be recalibrated at a later date (1992 Rev.Med.Suisse. Romande 112 775). However this is a technically difficult and potentially complicated ‘last ditch’ procedure that can only be recommended for consideration by those with an appropriate breadth of sub-specialist surgical expertise - if this fails then there is nothing much left to reconstruct (as with the occasional TVT erosion of the mid-urethral sphincter). The practical details of this posterior reduction sphincteroplasty are meticulously illustrated in chapter 9 of FRFUT - this is quite distinct from the ‘Young-Dees’ procedure for ectopia vesicae which is an anterior trans-pubic-gap reconstruction that predominantly relates to the bladder neck mechanism (a relatively unreliable sphincter at the best of times). However, as with this epispadiac procedure, the results of posterior-reduction-sphincteroplasty are much less successful when it has to be used in an endeavour to reconstruct the developmental sphicteric deficiencies of a female hypospadiac urethra.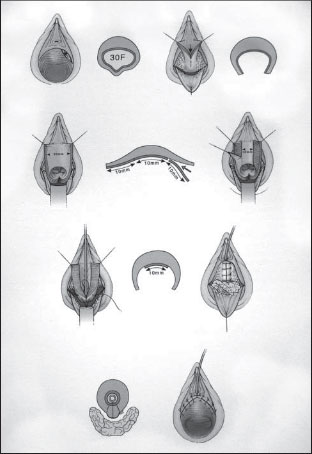
The T.W Posterior Reduction Sphincteroplasty.
I have received very much more than my fair share of honors. I was elected an honorary visiting urological surgeon to the Royal Prince Alfred Hospital Sydney in 1975, operating widely in Australasia annually until 1995 – and I was invited to more than 100 operating visiting professorships in the States, Canada and Europe. I served on both the Council of the RCS and the Council of the RCOG, was President of BAUS in 1988 and also appointed a Commander of the British Empire (CBE) by the Queen for ‘services to surgery’. I was elected an Honorary Fellow of both the Royal Australasian College of Surgeons and the American College of Surgeons - and both Margaret and I received an Honorary Doctorate of Science in New York in 1985. Uniquely, I have the special honor to be the only non Australasian of the twelve Fellows of the Australasian Urological Society and the only non American of the ten Honorary Fellows of the AAGUS. Great honors all – truly a fairy story and my cup overfloweth.
It has been the greatest fun and pleasure to have worked so closely with so many colleagues and friends - if indeed what we did is really ‘work’. Retirement is quite splendid - one of the special pleasures is still having many things to do, but not having to decide what one is going to do today until after a leisurely breakfast. Time stretches out delightfully for the time being - with a lovely garden in Exeter to enjoy with Margaret where we grow most of our own fruit and vegetables. In between times I can cast a fly for trout on the hallowed water of the Houghton Club on the River Test any day during the season – or perhaps fly our prewar Tiger Moth biplane with my godson Nick Parkhouse, a plastic surgeon. Utopia!
Richard Turner-Warwick, CBE
4886
© The Canadian Journal of Urology™; 16(6); December 2009

