 Indexed in Index Medicus and Medline
Indexed in Index Medicus and Medline
Free Articles
HOWIDOIT
The prone ureteroscopic technique for managing large stone burdens
Kevan M. Sternberg, MD,1 Bruce L. Jacobs, MD,2 Benjamin J. King, MD,1
Jared B. Wachterman, MD,1 Khaled Shahrour, MD,2 Katherine M. Theisen, MD,2 Sarah E. Sprauer, MD,2 Erin Ohmann, MD,2 Timothy D. Averch, MD2
1Department of Surgery, Division of Urology, University of Vermont, Burlington, Vermont, USA
2Department of Urology, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania. USA
STERNBERG KM, JACOBS BL, KING BJ, WACHTERMAN JB, SHAHROUR K, THEISEN KM,
SPRAUER SE, OHMANN E, AVERCH TD. The prone ureteroscopic technique for managing large stone burdens. Can J Urol 2015;22(2):7758-7762.
Percutaneous nephrolithotomy (PCNL) is the standard treatment for patients with large stone burdens, but can be associated with significant complications. Flexible ureteroscopy is an alternative approach that is less invasive, but often requires multiple procedures. Typically, many factors play a role in the decision to perform PCNL or ureteroscopy. The challenge is that it is difficult to predict which stone burdens will be able to be cleared ureteroscopically. We describe our approach using initial prone ureteroscopy with the transition to standard prone PCNL if required.
Key Words: percutaneous nephrolithotomy (PCNL), prone ureteroscopy, ureteroscopy, renal calculi, shock wave lithotripsy (SWL)
Percutaneous nephrolithotomy (PCNL) is the gold standard for large stone burdens and staghorn calculi due to its superior stone clearance and acceptable low morbidity compared with shock wave lithotripsy (SWL) and ureteroscopy.1 However, PCNL is not ideal for all patients with complex renal calculi; it is often deferred in cases of morbid obesity, pregnancy, coagulopathy, significant cardiopulmonary disease, and patient reluctance.2
Complications related to access and stone treatment can occur with PCNL. These include extravasation (7%), transfusion (11%-18%), and fever (21%-32%). More severe complications, such as sepsis (0.3%-5%), colonic injury (0.2%-0.8%), and pleural injury (0.0%-3%), occur less frequently.3
Flexible ureteroscopy with laser lithotripsy has been used with increased frequency to treat patients with contraindications to PCNL and to potentially reduce associated complications. With the availability of smaller ureteroscopes and small caliber holmium laser fibers, the intrarenal collecting system is easily accessible and the safe and efficient treatment of stones ureteroscopically is now routine.4 Single and staged flexible ureteroscopy has been shown to be an effective treatment for large (> 2 cm) and multiple renal calculi.5-7 Challenges to ureteroscopy, however, include a primary lower pole stone burden, a narrow infundibulo-pelvic angle, and matrix or infected stone debris.7,8
How we came to our current practice
We use prone split-leg positioning for all PCNL procedures. We have found this set up to be advantageous due to the ability to position the patient once for all portions of the procedure as well as assisting in obtaining renal access. For example, when stone burdens preclude getting a wire from the accessed calyx down the ureter, we have used a flexible ureteroscope to clear out obstructing calculi and pull the wire down the ureter. We have also used the flexible ureteroscope in difficult cases to select the desired posterior calyx and guide needle placement for access. With the ease of retrograde instrumentation in the prone split-leg position, an entire stone burden can be treated ureteroscopically while in the prone position.
At our institution, patients who may benefit from ureteroscopic treatment, but have lower pole stones or other factors making standard ureteroscopy more difficult, such as high stone density, are offered prone ureteroscopy. The advantage of prone ureteroscopy is that it allows for adjuvant PCNL without repositioning in circumstances where prone ureteroscopy alone is ineffective.
Between 2003 and 2013, 55 patients were scheduled for prone ureteroscopy by a single surgeon. Patients were counseled regarding the potential need for adjuvant PCNL in the same setting if it appeared that a purely ureteroscopic approach would not clear the stone burden. Patients with stone burdens of > 1 cm in size, lower pole stone location, and high Houndsfield units on preoperative CT were considered candidates for the prone ureteroscopic approach. We examined patient demographics, stone characteristics, and perioperative outcomes.
1) Patients receive either culture-specific or broad-spectrum intravenous antibiotics preoperatively.
2) After the administration of general anesthesia, the patient is positioned prone on a split-leg operating table. Rolls are placed from the axillae to the anterior superior iliac spines and the legs are gently flexed and spread. The split-leg table allows access to the urethra and therefore retrograde instrumentation throughout the case.
3) A flexible cystoscope is guided into the bladder and the trigone is identified. A 0.035 inch Bentson guide wire is guided into the ureteral orifice and passed up to the renal pelvis under fluoroscopic guidance. This is facilitated by looking up on initial entry to identify landmarks, making sure to not over distend the bladder, and by using an assistant to pass the wire into the orifice.
4) An 8 Fr, 10 Fr ureteral dilator set (Boston Scientific, Marlborough, MA, USA) is used to introduce a second 0.035 inch stiff body guide wire.
5) A ureteral access sheath (Cook, Bloomington, IN, USA) is placed over the stiff body wire under fluoroscopic guidance to the level of the uretero-pelvic junction and a flexible ureteroscope is then used to identify the intra-renal anatomy and evaluate the stone burden.
6) A 200 micron holmium laser fiber is used to fragment the stone burden and any sizable fragments are removed with a 0-tip basket (Boston Scientific, Marlborough, MA, USA). Stone fragmentation continues until either complete fragmentation was achieved or 3 hours elapsed. It is our protocol to stop procedures at 3 hours due to the increased risk of sepsis.
7) At the end of the procedure, a double J stent is placed under fluoroscopic guidance.
8) During prone ureteroscopy, if stone density, stone location, or renal anatomy is prohibitive, then percutaneous access is obtained. For this process, the flexible ureteroscope is used to guide needle placement, usually by locating a superior, posterior calyx.
9) The triangulation technique is used and an 18-gauge diamond-tip needle is directed fluoroscopically to the tip of the ureteroscope, entering at a 30-degree angle. The needle entrance is confirmed visually and, if needed, the wire can be guided down the ureter with the ureteroscope. In our experience, upper pole access allows treatment of the majority of the stone burden with the rigid nephroscope. If there is remaining stone, it can usually be reached with flexible nephroscopy.
10) Once percutaneous access is obtained, stone fragmentation and removal is achieved by using the lithoclast-ultra through a rigid nephroscope, a flexible scope with holmium laser lithotripsy, or a combination of the two.
11) Upon completion, a double J stent is placed, and a nephrostomy tube is left if there is concern for bleeding or residual fragments, necessitating a “second-look” procedure. Stone-free status is defined as the absence of any radio-opaque calculi on a combination of post-procedure fluoroscopy and postoperative imaging (e.g., an abdominal x-ray). Our decision- making algorithm and surgical steps are presented in Figure 1 and Table 1, respectively.
Of the 55 patients who underwent prone ureteroscopy, 41 (75%) were managed with ureteroscopy alone and 14 (25%) required adjuvant PCNL. The mean age of patients undergoing attempted prone ureteroscopy was 54 ± 14 years. Forty-five percent were men, and the mean body mass index was 30 ± 9 kg/m2. Most patients (65%) had a history of stone disease. The majority of patients (67%) had multiple stones and most were right sided (64%). The mean stone size was 2.1 ± 1.1 cm. Operative times for all cases had a mean of 126 ± 49 minutes. The average number of procedures required for the group was 1.6 ± 0.8. Overall, 33 (80%) were rendered stone free with prone ureteroscopy alone and 13 patients with adjuvant PCNL were stone free (93%). The stone-free rate of the cohort was 84%. There were no major complications with prone ureteroscopy alone and two major complications with adjuvant PCNL: one pulmonary embolism and one ICU admission for hypotension due to atrial fibrillation with rapid ventricular response.
PCNL remains the first-line treatment for large and complex intrarenal calculi.1 However, there has been increasing evidence that flexible ureteroscopy with holmium laser lithotripsy is effective for large stone burdens or multiple intrarenal calculi .5-7,9 The increased effectiveness of ureteroscopy is largely due to the advances in technology that have resulted in ureteroscopes with greater control and deflection.5
Debate exists over the efficacy of flexible ureteroscopy for large and multiple renal calculi. Schulham et al achieved an overall stone-free rate of 93% performing flexible ureteroscopy in 15 patients with a single calculus 2 cm or greater.5 The same group looked at 51 patients with a mean number of 3.1 renal stones treated with flexible ureteroscopy. Stone-free rates were 65% after one procedure and 92% after two procedures.6 Troxel et al used staged ureteroscopy for the treatment of renal stones larger than 2.5 cm. The average number of procedures required was 1.8, achieving an overall stone-free rate of 91%. They found that a significant lower pole burden was a limiting factor of this approach.7
The use of flexible ureteroscopy, as opposed to PCNL, for large stone burdens is attractive. First, flexible ureteroscopy can enable patients to avoid major complications associated with PCNL. These can result from the initial puncture and access of the collecting system (parenchymal bleeding, pleural injury, colonic injury, other intra-abdominal organ injury) as well as with stone disintegration and manipulation (septicemia, extravasation and fluid absorption from a perforated collecting system).3 Second, flexible ureteroscopy provides an opportunity for patients to be treated with a less invasive procedure that is less likely to result in hospitalization or absence from work.
Several factors must be considered in contemplating flexible ureteroscopy for large stone burdens. For example, a stone located in the lower pole may render ureteroscopy less effective in achieving a stone-free status.7 In addition, ureteroscopy may require multiple procedures to clear a large stone that may otherwise be completed with one PCNL session. In our group, 1.6 ureteroscopic procedures were needed to achieve a stone-free status. Other series have reported an average of 1.4 ureteroscopies to clear a large stone burden.5
Potential advantages of the prone ureteroscopic approach include the ability to convert to a percutaneous approach without repositioning the patient and the ability to approach a complex stone from both a retrograde and antegrade approach. Simultaneous ureteroscopy and PCNL has been shown to reduce the number of percutaneous tracts that would otherwise be needed for branched calculi or stones in unfavorable positions.10 In our cohort, 75% of patients avoided PCNL, suggesting a feasible alternative treatment for a select group of patients with large stone burdens.
Prone ureteroscopy is a safe and effective treatment option for a select group of patients with large renal calculi who would otherwise require a percutaneous approach. Patients treated with prone ureteroscopy alone avoid hospitalization and time away from family and work. A better understanding of what factors predict the use of prone ureteroscopy alone may help avoid the use of PCNL in a select patient population. Where prone ureteroscopy is unsuccessful, adjuvant PCNL can be performed without re-positioning, thus limiting potential complications to patient safety.
Accepted for publication February 2015
Address correspondence to Dr. Kevan M. Sternberg, Division of Urology, University of Vermont College of Medicine, Fletcher House 301, 111 Colchester Avenue, Burlington VT 05401 USA
TABLE 1. Procedure steps
| Steps | Tricks of the trade |
|---|---|
| Patient positioning: | |
| Prone split-leg table | Enables access to the urethra |
| Procedure: | |
| 1) Prone flexible cystoscopy | Look up to identify the trigone. Do not over distend the bladder. Use an assistant to advance the wire. |
| 2) Identify ureteral orifice and pass wires | |
| 3) Consider ureteral access sheath | Facilitates re-entry into the ureter, decreases intra-pelvic pressure. |
| 4) Prone flexible ureteroscopy, laser lithotripsy, stone extraction | |
| 5) Ureteral stent placement if stone burden cleared | |
| Intra-operative decision- unable to clear stone burden: | |
| 6) Convert to percutaneous nephrolithotomy if stone burden not cleared | No need to reposition. Ureteroscopic guidance or air pyelogram through ureteral occlusion balloon. |
| 7) Renal access into chosen posterior calyx | |
| 8) Introduction of wires | |
| 9) Balloon dilation | |
| 10) Rigid and flexible nephroscopy with lithotripsy and stone extraction | Lithoclast ultra, holmium laser, or combination. |
| 11) Placement of ureteral stent and possible nephrostomy tube | Nephrostomy tube left if concern for bleeding or residual stone requiring "second look" procedure. |
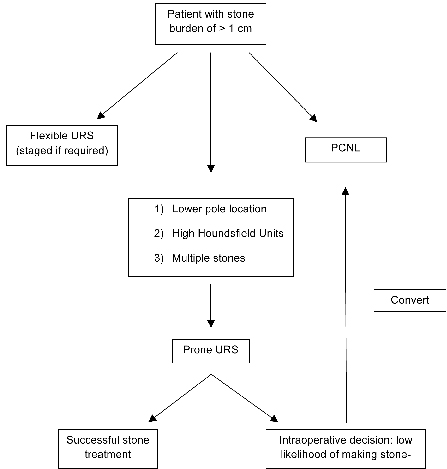
Figure 1. Treatment algorithm.
1. Preminger GM, Assimos DG, Lingeman JE et al. Chapter 1: AUA guideline on management of staghorn calculi: Diagnosis and treatment recommendations. J Urol 2005;173(6):1991-2000.
2. Hyams ES, Shah O. Percutaneous nephrostolithotomy versus flexible ureteroscopy/holmium laser lithotripsy: Cost and outcome analysis. J Urol 2009;182(3):1012-1017.
3. Michel MS, Trojan L, Rassweiler JJ. Complications in percutaneous nephrolithotomy. Eur Urol 2007;51(4):899-906; discussion 906.
4. Preminger GM. Management of lower pole renal calculi: Shock wave lithotripsy versus percutaneous nephrolithotomy versus flexible ureteroscopy. Urol Res 2006;34(2):108-111.
5. Breda A, Ogunyemi O, Leppert JT, Lam JS, Schulam PG. Flexible ureteroscopy and laser lithotripsy for single intrarenal stones 2 cm or greater--is this the new frontier? J Urol 2008;179(3):981-984.
6. Breda A, Ogunyemi O, Leppert JT, Schulam PG. Flexible ureteroscopy and laser lithotripsy for multiple unilateral intrarenal stones. Eur Urol 2009;55(5):1190-1196.
7. Riley JM, Stearman L, Troxel S. Retrograde ureteroscopy for renal stones larger than 2.5 cm. J Endourol 2009;23(9):1395-1398.
8. Grasso M, Conlin M, Bagley D. Retrograde ureteropyeloscopic treatment of 2 cm. or greater upper urinary tract and minor staghorn calculi. J Urol 1998;160(2):346-351.
9. Cohen J, Cohen S, Grasso M. Ureteropyeloscopic treatment of large, complex intrarenal and proximal ureteral calculi. BJU Int 2013;111(3 Pt B):E127-E131.
10. Marguet CG, Springhart WP, Tan YH et al. Simultaneous combined use of flexible ureteroscopy and percutaneous nephrolithotomy to reduce the number of access tracts in the management of complex renal calculi. BJU Int 2005;96(7):1097-1100.

