Introduction
Ileal conduit remains the most frequently utilized method of urinary diversion performed, after radical cystectomy.1 Since the ileal conduit was popularized by Bricker in 1950,2 it has become the gold standard in urinary diversion. Most often it is indicated in conjunction with radical pelvic surgery for malignancy.3 Despite subsequent enthusiasm for alternative techniques for continent diversion and orthotopic neobladder,4 recent studies have shown a significant trend back toward the more liberal use of the ileal conduit urinary diversion.1,5
Complications of ileal conduits remain an important concern in urologic surgery, and ureteroileal anastomotic stricture remains one of the most common late complications observed.6-8 As recognized early on by Bricker, stricture occurrence depends largely on the technique and care with which the ureter is anastomosed to the ileum.2 An anastomotic stricture is significant in that another procedure is usually required to treat the stricture in attempting to preserve renal function.8,9 These procedures include anastomotic stenting, percutaneous nephrostomy tube placement, balloon dilation, endoscopic incision, open anastomosis revision, and nephrectomy.9
While the standard Bricker anastomosis has the advantage of separating the upper tracts, some studies have shown a greater stricture rate than the Wallace conjoined ureteroileal anastomosis.3,10,11 However, others claim there is no significant difference.12,13
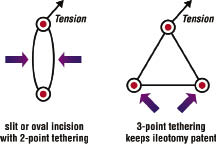
A linear slit incision or excision of a small oval of ileum has been described in creating the ileotomy.14-16 We hypothesized that utilizing a “shield shaped” rather than a standard slit ileotomy would reduce the incidence of anastomotic strictures. This hypothesis originates from the observation that the shield shaped ileotomy closely mimics the opening of the spatulated ureter, potentially minimizing suture line tension and gapping.
Ischemia of the distal ureter has been blamed for playing a role in the development of stricture at the anastomosis site. Tension caused by tunneling the left ureter below the sigmoid mesocolon has also been implicated as a possible factor in anastomotic stricture formation because left sided strictures have been observed more commonly.15,17,18 The latter etiology may be additionally relevant in a population with increasing obesity. In this proposed technique, a small triangular segment of ileum is excised, potentially inhibiting fusion of the ileal edges of the anastomosis.
We retrospectively reviewed the outcomes of one surgeon’s experience at a medium size tertiary state hospital performing initially a standard slit incision in 25 patients during 2001-2005, and subsequently a shield shaped incision in 25 patients during 2006-2009.
Materials and methods
A retrospective review of an IRB approved computerized surgery database was performed to identify patients who underwent cystectomy with construction of an ileal conduit urinary diversion by a single surgeon between 2001 and 2009. Each patient’s electronic medical record was reviewed for demographics such as age, gender, comorbidities, history of prior radiation or chemotherapy, and smoking history. Data on each patient was then obtained on date of surgery, type of ileotomy, indication, development of postoperative ureteroileal anastomotic stricture, date of diagnosis of stricture, imaging modality used to diagnose stricture, stricture treatment, outcome, and length of follow up.
All patients identified underwent a Bricker-type ileal conduit performed by a single surgeon. Senior or chief resident physicians actively participated as operative surgeon during all cases. In each procedure, a 15 blade scalpel with visual approximation was utilized to make a proximal ileotomy in the isolated length of ileum using either: 1) a standard slit incision or 2) a triangular shield shaped incision. The distal ureter was spatulated using Potts scissors and a retention suture was used to minimize handling of the ureter. A double-armed suture (5-0 long acting absorbable monofilament [Maxon]) was utilized to make a running closure of the anastomosis starting at the apex of the spatulated ureter where an initial knot was tied. See Figure 1.
The suture was locked at each remaining corner of the triangle and then continued to completion of the anastomosis. A 6-7 French single-J stent was placed prior to final closure and the distal end brought out through the stoma. Stents were removed 2-3 weeks postoperatively without imaging. A Jackson-Pratt drain was routinely left after each procedure and removed after a drain fluid creatinine was obtained to confirm no anastomotic leak and the patient was tolerating an oral diet. Stents were removed 2-3 weeks postoperatively without imaging. There was no difference in technique between the procedures other than variance in the type of ileotomy incision made at the site of ureteroileal anastomosis. One patient in each group survived less than 90 days postprocedure and was excluded.
Continuous data were summarized using the mean, standard deviation (SD), and range. The two sample t-test was used to compare the two groups in terms of age. Fisher’s exact test with mid-p correction was used to compare the two groups in terms of categorical variables. Exact methods were used to estimate the odds ratio for the comparison of the two groups in terms of the incidence of ureteroileal anastomotic stricture. Mantel-Haenszel analysis was used to account for the effect of confounding variables. All significance tests were two-tailed and a significance level of 0.05 was used throughout.
Results
A total of 50 patients underwent Bricker ileal conduit construction between 2001 and 2009. Of these cases, 48 were known to survive beyond 90 days postprocedure. Group 1 consisted of 24 patients (48 renal units) who underwent a standard slit incision ileotomy from 2001 through 2005. Surgical indications for Group 1 included transitional cell carcinoma (20), bladder sarcoma (1), refractory radiation cystitis and hematuria after pelvic radiation for prostate cancer (1), pelvic exenteration for rectal cancer (1), and paraplegia with a vesicovaginal fistula (1). Group 1 demographics showed a mean age of 63.7 years (SD 12.2), 83% male, 12.5% diabetes, 66.7% hypertension, 83.3% with smoking history within past 35 years, 16.7 % prior radiation, and 20.8% prior chemotherapy history.
Group 2 consisted of 24 patients (47 renal units) who underwent a shield shaped ileotomy from 2006 through 2009. Surgical indications included transitional cell carcinoma (20), pelvic Ewing’s sarcoma (1), refractory CIS of the bladder and prostate (1), intractable radiation cystitis after pelvic radiation for prostate cancer (1), and kidney transplant (solitary) requiring an ileal conduit creation. Group 2 demographics showed a mean age of 60.9 years(SD 15.0), 79% male, 20.8% diabetes, 83.3% hypertension, 62.5% with smoking history within past 35 years, 12.5 % prior radiation, and 29.2% prior chemotherapy history. See Table 1.
A total of 95 renal units were anastomosed. From these, a total of 8 (8.3%) ureteroileal anastomotic strictures were identified: 6 of 48 renal units (12.5%) in Group 1 and 2 of 47 renal units (4.2%) in Group 2, Table 2. Statistical analyses showed a p value of 0.17 and odds ratio of 3.21. In Group 1, a patient had stricture of both ureters detected 1 month apart. Stricture diagnosis in this cohort occurred at 1, 4, 4, 5, 14, and 42 months after surgery. The latter patient initially had bilateral hydronephrosis identified about a month after surgery. One side resolved, but she was subsequently lost to follow up for 3 years, leading to a delay in stricture diagnosis by IVP and Mag-3 renal scan at 42 months. In Group 2, strictures were diagnosed at 6 and 10 months after surgery.
Because of the lower frequency of smokers and those with prior radiation treatment among those in Group 2, a stratified analysis was performed to account for these differences, Table 3. Interestingly, all 6 patients with a ureteroileal anastomotic stricture in Group 1 were smokers, whereas neither of the 2 patients with a stricture in Group 2 were smokers. Accounting for the lower frequency of smokers and prior radiation treatment in Group 2 had no material effect on the estimated odds ratio of 3.21 when comparing Groups 1 and 2 (odds ratio = 3.27 after accounting for smoking, 3.05 after accounting for prior radiation treatment).
Mean follow up time was 24.2 months (2 to 85 months) and 12.3 months (2 to 26 months) for each group, respectively. In Group 1, 5 patients had less than 6 months’ follow up. Two had developed early postoperative metastasis and were placed on hospice care, 2 sought follow up with their local urologist due to the distance from our academic center, and 1 was a quadriplegic managing issues of multiple sacral decubitus ulcers and lost to follow up at
4 months. Group 2 also had 5 patients with follow up less than 6 months. Two were discharged to hospice with metastasis, 1 died of rapidly progressive disease 4 months after surgery, and 2 are recent cases with current continuation of follow up.
Radiologic imaging techniques used to identify or confirm strictures included intravenous pyelogram (IVP), Mag-3 renogram, loopogram, and abdominopelvic CT scan. Stricture treatment included four kidneys with percutaneous nephrostomy tube (PCNT) placements (two were in 1 patient with bilateral ureteral strictures) and these individuals were discharged to hospice with indwelling PCNT due to metastasis. There were also three nephrectomies (of which one had a coincidental renal mass on the same side as the stricture), one endoscopic dilation, and one patient elected observation.
After 10 cases, it became our routine practice to obtain a drain creatinine during the first 4 postoperative days to assist with timing of drain removal. There was no increase in postoperative anastomotic leakage. Creatinine levels were elevated in 8.3% and 4.2% of Jackson-Pratt drains in Groups 1 and 2 respectively, despite lack of data from the initial 10 patients’ in Group 1. None of these patients developed a clinically significant leak and all resolved with conservative management within 2 weeks. Six (75%) of the total eight ureteroileal anastomosis strictures were on the left and two (25%) were on the right side.
Discussion
There are several potential etiologies for ureteroileal stricture formation. Ischemia of the distal ureter due to prior radiation therapy, during surgical dissection, or mishandling of the distal ureter has been blamed. Disease progression and separation of the anastomosis with subsequent scarring and adherence/fusion of the ileotomy mucosal edges are additional potential causes of stricture. Tension caused by tunneling the left ureter below the sigmoid mesocolon has also been implicated as left sided strictures have been observed more commonly.15,18 This was also the case in our study group. The latter etiology may be of additional relevance in an increasingly obese population.
It is interesting to postulate that the shield shaped ileotomy may provide for three points of tethering at the corners of a triangle, Figure 2a. Tension in one direction on a slit or oval incision which has two points of tethering may pull the ileotomy and ureteral edges together, Figure 2b. A shield shaped anastomosis triangulates the suture line, providing three points of tethering when under tension. This potentially maintains an open lumen during the period of healing.
The use of a triangular anastomosis to improve patency of a lumen was pioneered by Alexis Carrel in end-to-end and end-to-side microvascular anastomoses of transplant organs in the early 20th century.19 Two prior ileotomy techniques have been described when creating an ileal conduit, the slit and oval ileotomy.15-17 To our knowledge, a triangulation method has not been described before for use in performing a ureteroileal anastomosis.
Although tension has been implicated in stricture formation, ischemia remains an important issue. Avoiding ischemia of the distal ureter is pertinent in preventing stricture formation. Careful dissection while minimizing handling of the distal ureter (i.e., utilizing a retention suture) is always essential to prevent ischemia.
Modifying the ileotomy from a standard slit to a shield shaped incision did not eliminate the occurrence of postoperative anastomotic strictures. Of note, there was concern for, or diagnosis of, all strictures by 14 months. This pilot study has shown that the shield shaped ileotomy results in a similar or potentially slightly lower stricture rate compared to a slit incision. This study’s finding did not reach statistical significance (p = 0.17) because of the small sample size. An odds ratio of 3.21, however, is indicative of a clinically meaningful decrease in the incidence of anastomotic strictures when comparing the standard slit incision to the shield shaped ileotomy. These results suggest that future studies with a larger cohort are needed.
Our study suffers from the limitations of a sequential cohort retrospective series and from the associated shortcomings of being a sole state tertiary medical center in a largely rural state. Follow up has been inconsistent often due to patient mandate or preference to follow up closer to their area of residence. In Group 1, four patients were lost to follow up either because their disease appeared stable or because of distraction from other health issues. Group 2 had one patient lost to follow up but follow up time is limited in this group, in particular for recent patients in this shield-type incision cohort. That said, an identical number in each cohort (5) have follow up of less than 6 months.
Learning curve of the surgeon may contribute to a decreased stricture rate. All anastomoses, however, were performed by senior or chief residents during their respective rotations under the tutelage of the attending surgeon.
During our tutelage of this technique, we have subjectively found that this surgical modification allows for easier suturing as the spatulated ureter is separated or splayed open compared to anastomosing to an ileal slit incision. The suture line becomes easily visible and thus anastomosis is technically easier to perform. This technique also did not result in an increase of anastomotic extravasation.
Conclusion
Modifying the ileotomy from a standard slit to a shield shaped incision does not eliminate postoperative anastomotic strictures. A possible decrease in stricture rate will need confirmation with longer follow up and larger study groups. This surgical modification did not result in anastomotic extravasation and we believe it is technically easier to perform.

 Indexed in Index Medicus and Medline
Indexed in Index Medicus and Medline